IUD Insertion
IUDs
Long-acting, immediately reversible, and highly effective (99.2–99.8%), the intrauterine device (IUD) is recommended as a first-line method of contraception. It is an excellent option for youth, adolescents, adults, immediate postpartum use, and later reproductive years, including peri-menopausal women experiencing abnormal periods.
Hormonal IUDs are also commonly used for cycle control in women struggling with heavy or painful periods, and they provide endometrial protection in women using menopause hormone therapy (MHT).
One of the greatest benefits of an IUD is that its effectiveness does not depend on daily or routine action by the user. Once placed, you can simply forget about it — it is discreet, reliable, and cost-effective.IUDs can also serve as emergency contraception when inserted within seven days of unprotected intercourse.
Since many family physicians do not provide IUD insertions, we are here to offer expert care and support throughout the process.
IUD Basics
The IUD is a small, soft T-shaped device that is inserted into your uterus, also known as your womb, to prevent pregnancy.
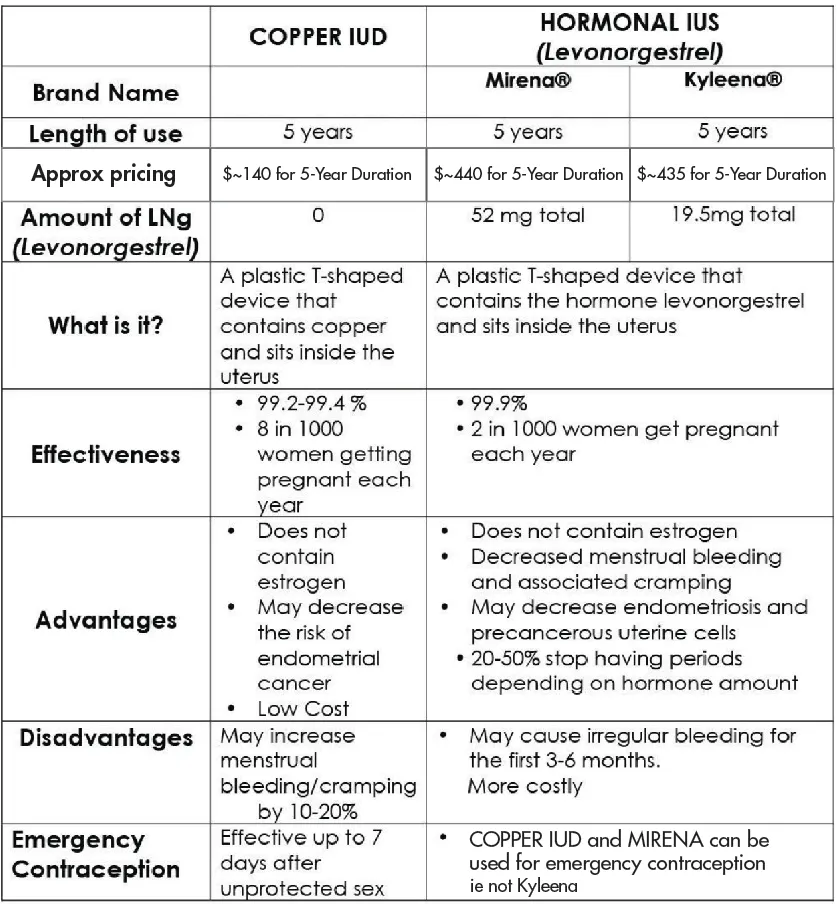
Some IUDs contain a hormone (Mirena and Kyleena LNG IUS) called progesterone which can reduce menstrual bleeding or stop menstruation altogether.
Whereas , Copper IUDs , are hormone free and the top choice for women who want to avoid hormones.
Let’s sit down and see what best suits your lifestyle.
How effective is an IUD?
An IUD is one of the most effective contraception methods – it is 99% effective and lasts between 3 to 8 years, depending on the type.
Types Of IUDs Offered In Our IUD Clinic in Langley
There are two styles of IUDs available in Canada.
Hormonal IUDs:
Mirena® and Kyleena® are hormonal (progesterone-based) IUDs that are completely free of estrogen.
Mirena® provides contraception for up to 8 years and is also approved for the management of heavy or painful periods.
Kyleena® lasts for 5 years and is used primarily for birth control.
Both IUDs release a small, steady amount of levonorgestrel, a hormone similar to progesterone which your body naturally makes. This works by:
Thickening the cervical mucus to block sperm.
Thinning the uterine lining, which makes periods lighter or may even stop them completely.
Because of these effects, hormonal IUDs are often a great choice for women with heavy or painful periods, athletes, or anyone who prefers to avoid monthly bleeding.
IUD's can be removed at any time, are safe to use while breastfeeding, and do not affect future fertility—your ability to become pregnant returns quickly after removal.
2. Copper IUD is the only form of birth control that is completely hormone-free, making it an excellent option for any women who prefer to avoid hormones. This includes breastfeeding mothers or women with depression or anxiety who wish to avoid hormonal effects on mood.
Copper IUDs are available with a lifespan of 3, 5, or 10 years, depending on the style. The device consists of a small, flexible piece of plastic shaped like a “T,” with copper wrapped around it — which is why it is called a copper IUD.
The copper is released into the uterine cavity, preventing pregnancy by stopping sperm from fertilizing an egg and reducing sperm movement. It also thickens the cervical mucus, forming a barrier that prevents sperm from entering the uterus.
Because copper IUDs may make periods longer, heavier, or more painful, particularly during the first few cycles. In most cases, this settles over time, but if heavier or painful bleeding persists beyond six months, it is unlikely to change after that and you should speak to your healthcare provider as heavy periods can lead to iron deficiency and anemia
IUD Insertion
For women who have never been pregnant, scheduling the IUD insertion during or just after your period can make the procedure easier and more comfortable, although Dr. Gerber can insert an IUD at any time during your cycle.
To help ensure your comfort, a local anesthetic ( cervical block) is used to numb the cervix during the procedure.
For patients who may need additional support, we also offer oral sedation (Ativan/lorazepam) or inhaled anesthesia (Penthrox/methoxyflurane, commonly called the “green whistle”) in select cases to help manage anxiety and pain. If you think you may need these methods, a phone consultation is required before your appointment.
The IUD insertion procedure typically takes less than five minutes.
Dr. Gerber uses breathing techniques to help make the process easier, and local numbing or freezing . The IUD is inserted into the uterus using sterile instruments.
Pain experience varies from person to person. Some patients feel only a mild pinch or cramping similar to menstrual discomfort, while others may experience more intense cramping .
Most patients find the procedure " not as bad as they were expecting."
To help ensure the procedure goes smoothly, arrive well prepared: take Naproxen 440 mg when you arrive at the clinic, be well hydrated, and have eaten something light. If you anticipate you might be sensitive to procedures, it is recommended to arrange for a ride home afterward.
It is important to be cautious about information on social media. Many patients who have positive experiences do not share them, while negative or exaggerated stories are often more visible. Most patients manage the procedure well with Naproxen and local anesthetic (cervical block), and social media posts may not accurately reflect the typical experience.
Using social media as a reference often creates unnecessary anxiety and misinformation.
IUD Care
Most women are able to return to work immediately after the procedure. At our clinic, we recommend that for the first 24 hours following an IUD insertion , you avoid placing anything inside the vagina to reduce the risk of infection. During this time, use pads or panty liners and take showers rather than baths. After the first 24 hours, you can resume all normal activities, including swimming, using hot tubs, and inserting menstrual cups or tampons.
MIRENA or KYLEENA IUDs become effective 7 days after insertion. If you weren't using birth control prior to the procedure, we recommend using condoms or avoiding sex during the first week. If you were using the pill, patch, or ring, continue using that method for 7 days or refrain from sex during the first week.
Copper IUDs Copper IUDs are effective immediately after insertion and do not require an overlap with other forms of contraception, such as condoms.
If you experienc low grade cramping after the procedure take Ibuprofen or Tylenol or use a heating pad.
IUD STRING CHECKS: Checking your IUD threads is optional but can provide reassurance that your IUD is in place and functioning properly. To check, gently insert your middle finger into the vagina until you reach the cervix, which feels firm and rubbery. The IUD threads should be coming out of the cervix.
Many women find it difficult to feel the strings at first, so some practice may be needed. You can try different positions or ask your partner to help feel for the strings.
If you are concerned, use condoms, take a pregnancy test, and contact your doctor or a walk-in clinic for a string check.
Never pull on your IUD strings, as this can cause the IUD to shift or fall out. Regularly checking the strings is optional, but it can help detect if your IUD has moved. IUDs may shift during the first few months after insertion or during a menstrual period. If the strings feel longer or shorter than usual, or if you feel the hard part of the IUD against your cervix, the IUD may have shifted. In this case, use condoms and contact your healthcare provider.
IUD Removal
When you choose to change contraception methods, plan a pregnancy, replace your expiring IUD or simply discontinue use, the IUD can be easily removed at our clinic.
To prevent any chance of pregnancy, you should either abstain from vaginal intercourse or use condoms for at least one week before IUD removal.
If you plan to switch to another contraceptive method, such as the pill, patch, or ring, it is ideal to start your new method seven days before your IUD removal appointment.I
IUD removal is generally a straightforward procedure that typically involves only mild cramping. Sterile instruments are used to grasp the threads and gently slide the IUD out of the uterus.
If the IUD threads cannot be seen, the removal may be more complicated and require additional instruments and local numbing or freezing to locate the IUD. In rare cases, if the IUD cannot be removed in the office, a referral to a gynecologist may be necessary, and minor surgery may be required to remove the device.
Pain and Anxiety Management Options for IUD Procedures
We understand that IUD insertion and IUD removals (where strings can't be seen) can cause discomfort or anxiety for some patients. To make the experience as comfortable as possible, we offer several options to help manage pain and anxiety, although most patients do well with oral analgesics and local anesthesia alone.
1. Oral Analgesics
Medications such as naproxen (available over the counter as Aleve) can help reduce general discomfort and inflammation associated with IUD procedures. Taking naproxen 500 mg or Aleve 440 mg about an hour before your appointment can minimize cramping and pain during and after insertion or removal.
Studies have shown that naproxen is more effective than Tylenol (acetaminophen) or ibuprofen (Advil) for managing this type of discomfort.
2. Cervical Block (Local Anesthetic Injection)
A cervical block involves injecting a local anesthetic, such as lidocaine, directly into the cervix. This method effectively numbs the area and can significantly reduce pain during the procedure, making the experience much more comfortable. Injecting in the cervix for most patients feels like a pinching or pressure sensation and unlike getting a needle in your skin.
A cervical block is not usually needed in women if the cervix is already soft and open, or in women with multiple natural births , freezing usually offers no additional benefit, Our approach is to use only what is necessary for safe and effective insertion.
3. Topical Anesthetic (Benzocaine Spray)
We do not use topical sprays as they are not effective .
4. Inhaled Anesthetic Gas (Penthrox / Methoxyflurane = Green Whistle )
Penthrox is an inhaled anesthetic that helps manage both pain and anxiety. Administered through a hand-held, single-use inhaler, it allows patients to self-administer and control their dosage. Methoxyflurane works quickly to relieve pain while providing a calming effect, making the procedure more tolerable. Most patients tolerate Penthrox well although possible side effects include drowsiness, dizziness, nausea, headache, lightheadedness.
Penthrox is suitable for adults ( 18 years and older) in good general health and able to self administer it. If you are prescribed this option, avoid eating a heavy meal beforehand .
Penthrox is not a benefit of MSP and will cost you approximately $100.
Penthrox is not suitable for all patients, and is not approved for patients under 18 years of age. Please inform us before your appointment if this is something you are interested in as a consultation is required before its use. During this consultation, we will review your medical history, allergies, and a complete list of your current medications to ensure safety.
Important : Patients choosing this option must arrange a ride home, as you should not drive or operate heavy machinery for 24 hours after use.
5. Oral Anxiety Medication (Ativan / Lorazepam)
For patients experiencing significant anxiety, oral Ativan (lorazepam) can be taken prior to the procedure. While it does not directly relieve pain, reducing anxiety can help patients manage discomfort more effectively.
Important: A consultation is required before using Ativan . Patients must arrange a ride home and should not drive or operate heavy machinery for 24 hours following the procedure.
Frequently Asked Questions
- There are two styles of IUDs available in Canada:
Hormonal progesterone-based IUDs (Mirena and Kyleena) continuously release low levels of levonorgestrel, which is a progestin much like the hormone progesterone produced by the ovaries. Levonorgestrel thickens cervical mucous, so sperm and ovum do not meet. It also thins the lining of the uterus, making it an excellent choice for women with heavy periods.
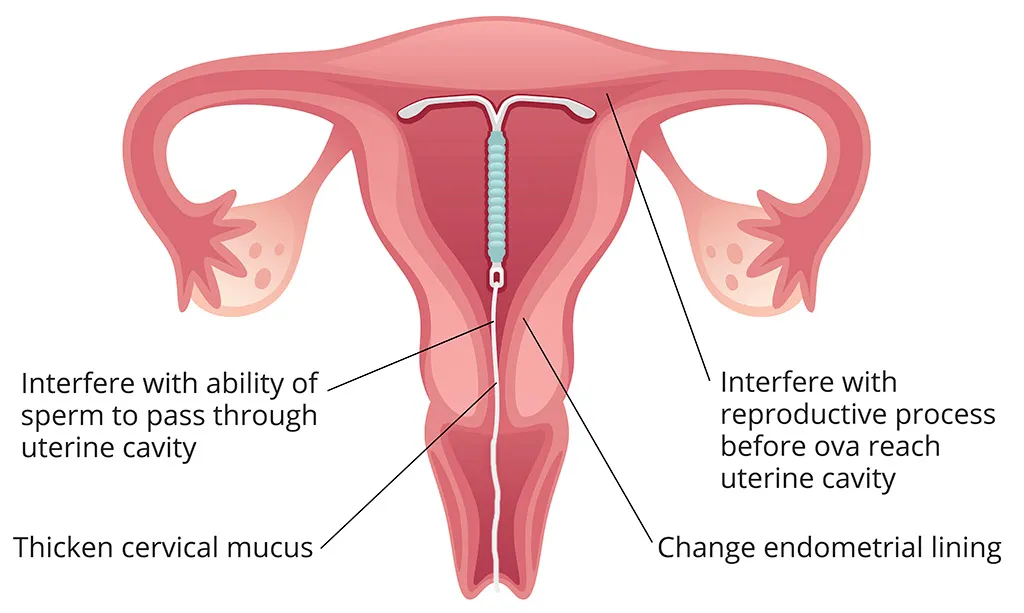
- Non-hormonal /copper-based IUDs release copper into the uterus and prevent pregnancy by stopping sperm from fertilizing an egg and reducing sperm movement.
- IUDs are Estrogen free. This reduces your risk of a blood clot
(Smokers should avoid estrogen containing contraception). - IUDs have less hormonal side-effects than the pill, patch or ring which contain both estrogen and progesterone.
- IUDs are safe for breastfeeding.
- IUDs do not cause hormone-related facial pigmentation like chloasma or melasma.
- An IUD provides long-term contraceptive protective for five to 10 years, which makes it the cheapest form of birth control available.
- You cannot forget it, skip it or mess it up. As long as it is in position in the uterus it works.
- It is also convenient, as you do not have to remember to take pills or apply patches or rings regularly.
- Because the IUD cannot be seen or felt, it is private. It is your choice to share information about the IUD.
- In 60% of women using Mirena, menstrual flow becomes lighter or can stop altogether. It is an excellent treatment for women with heavy and or painful periods.
- IUDS are very reliable birth control for women who are not allowed to get pregnant due to medical reasons including women taking Accutane for acne.
- When you are ready to become pregnant, your healthcare provider can easily remove the IUD by pulling on the strings with no long-term effects on your fertility or future pregnancies . IUDs do not stop ovualtion, so return to fertility is immediate.
- IUDs can be used for Emergency contraception ( if placed within 7 days after unprotected sex eg. broken condom.
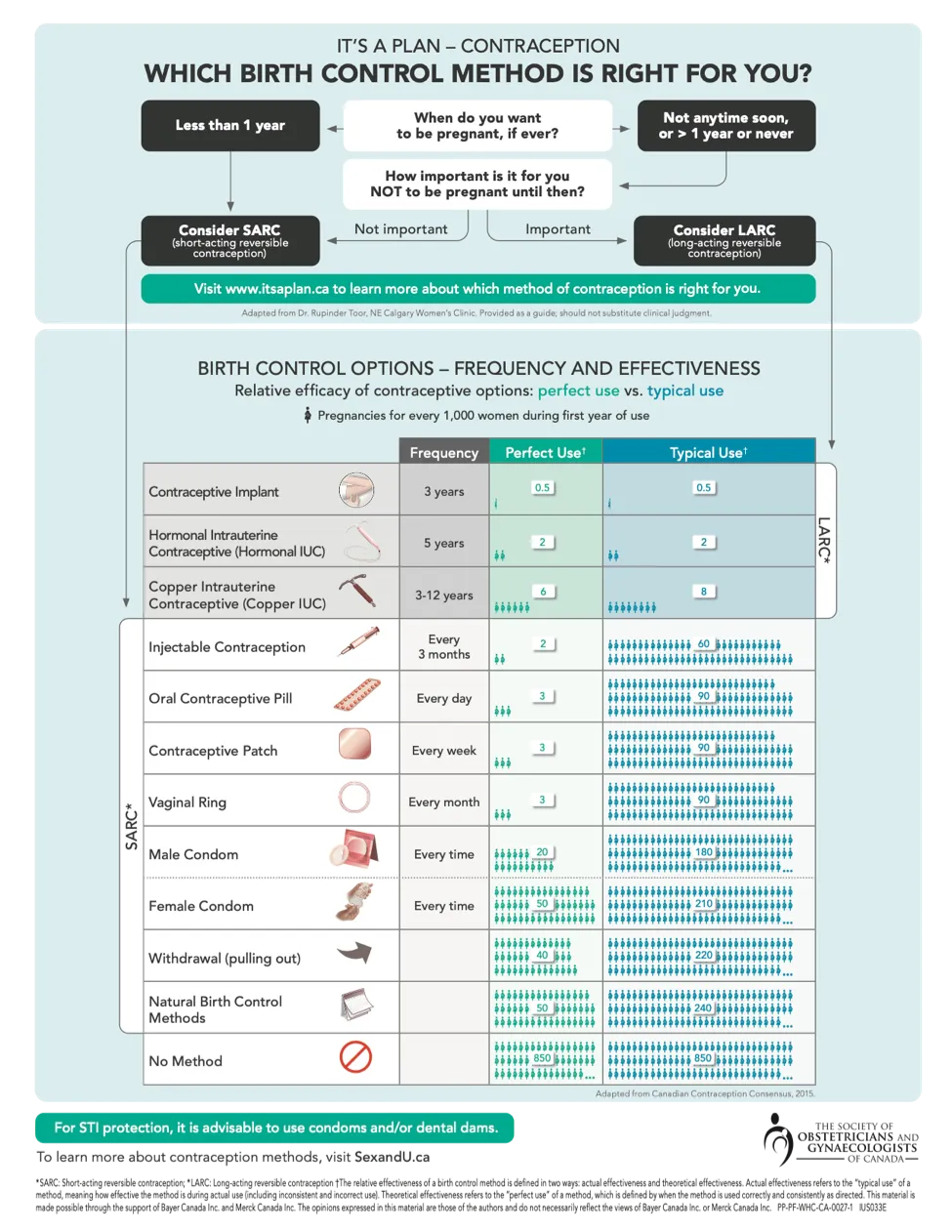
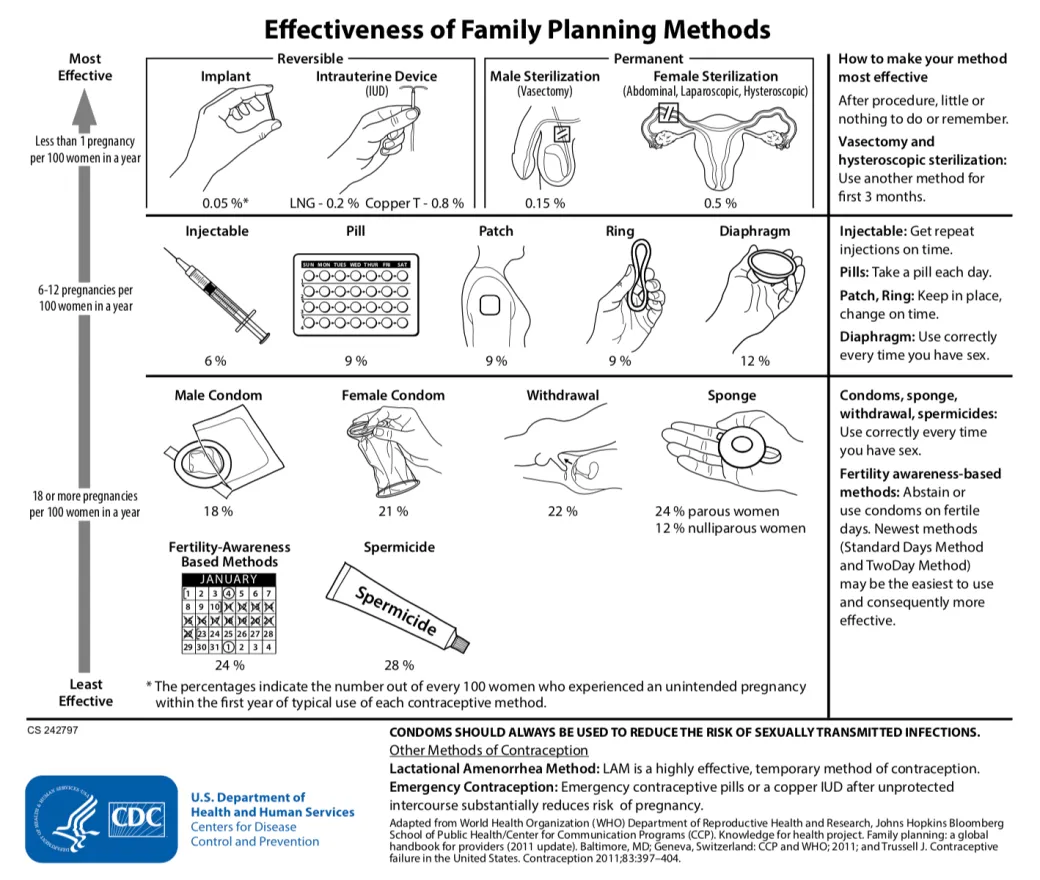
- The above chart shows the number of pregnancies for each method. Perfect use is derived from clinical trials and does not represent real-life outcomes. Typical use failure rates are real to life.
- No.
Hormonal IUDs can be used to improve quality of life by reducing menstrual flow in women with heavy bleeding and to improve painful periods. - Hormonal IUDs improve Iron deficiency anemia in women with heavy periods.
- Hormonal IUDs can be used to manage pain and bleeding in patients with endometriosis.
- Many athletes who do not want their periods get hormonal IUDs.
- IUDs are very reliable for women who have medical reasons that don’t allow pregnancy, such as women taking Accutane for the treatment of acne.
- Copper IUDs are great for women who can not tolerate hormonal birth control as they are hormone free.
- Certain Copper IUDs and Mirena IUD can be used for emergency contraception if placed within 7 days of unprotected sex.
- No. With hormonal IUDs, the lining of the uterus generally does not thicken, so does not need to be shed (that is your period).
- In fact, the progestin released from hormonal IUDs inside the uterus, protect against abnormal cell changes in thelining that could lead to uterine cancer.
- In 60% of women using Mirena, menstrual flow might become lighter or stop altogether. By the 6th month, 1 in 5 women with MIRENA no longer menstruate, making it an excellent option for women with heavy periods.
- Many. You don’t have to remember to take it, and it is a discrete, private choice.
- IUDs are a good choice for women who have an increased tendency to blood clotting, including deep vein clots, or pulmonary embolism eg. women who smoke nicotine.
- They work for 3-5-10 years (depending on the style) which makes them the most cost-effective method of birth-control.
- IUDs are also easy to remove should you wish to become pregnant, with no long-term effects on your fertility or future pregnancies.
- Hormonal IUDs can benefit women with endometriosis (redue pain and bleeding) and irregular periods (polycystic ovarian disease).
- IUDs have been shown to reduce the risk of uterine and cervical cancer.
- IUDs do not protect against sexually transmitted infections. Always use condoms for STI protection.
- Hormonal IUDs may cause irregular bleeding and spotting, which can take several months to settle because the uterus can take time to adjust to the hormones. This is not serious and requires patience.
- About 10% of women with hormonal IUDs have them removed for hormonal side effects like acne, weight gain or mood changes.
- Copper IUDs may cause heavier, longer and/or more painful periods, but this typically improves within a few months. Women with heavy and or painful periods should avoid Copper IUDs, as it could worsen your symptoms.
- Women with low iron should also avoid copper IUDs.
- Rarely (< 1% ) the IUD can :
injure (perforate) your uterus wall—this is not serious and heals on its own. It will not cause any problems later with fertility. - fall out (expulsion) - this is more commeon if an IUD is placed in the post partum period (after a baby).
- moves outside the uterus (migration) - in this event minor surgery is required to remove the IUD
- When your doctor inserts the IUD inside the uterus, the strings, made of plastic threads, are cut about 2 cm from the cervix.
- To check them, first, wash your hands. Then, while sitting or squatting, insert your index or middle finger into your vagina until you touch the cervix, which will feel firm and rubbery. Feel for the IUD string ends coming through your cervix. If you feel the strings, it is in place and should be working.
- If the strings feel longer or shorter than the last time you checked them, or if you feel the hard part of the IUD against your cervix, your IUD may have moved. In this instance, you should use condoms and see a doctor. Do not try to push the IUD back yourself. Also, never pull on the IUD strings.
- If you're worried your IUD has moved, use backup birth control until you can see your doctor. Perform a home pregnancy test to exclude pregnancy. If your doctor cannot locate the strings during a pelvic exam, she may order imaging tests like a pelvic ultrasound to confirm the location of the IUD.
- It is rare for your IUD "to move out of place" if properly placed by a skilled inserter. If this does happen it usually occurs in the first few months. Symptoms that could indicate your IUD is malpositioned include abnormal bleeding or pelvic pain .
- Usually, they have tucked themselves into the cervical canal or uterus. The strings can be easily swept back into view by your doctor during a pelvic exam using a device called a cervical cytology brush. Sometimes, a pelvic ultrasound is useful to confirm your IUD is in the womb.
- Missing strings might be a sign that the entire device has " fallen out " from the uterus. This is very rare but reinforces the need to check your strings regularly.
- Sometimes a partner can feel the strings, so you may wish for them to be cut shorter. Once cut, it can be challenging to check for strings and you will need to be seen by a skilled health-care provider when your IUD is due for removal or you desire pregnancy.
- No. Your IUD will continue to work just as effectively, regardless of how many sexual partners you have.
- This happens rarely. If it does, have the IUD removed as soon as possible.
- If you choose to change contraceptive methods, wish to plan a pregnancy sooner or discontinue use, an IUD can be easily removed by a healthcare professional. It is usually a simple process done by inserting a speculum and using the threads to slide the IUD out from the uterus through the cervix. Some experience brief cramping during removal.
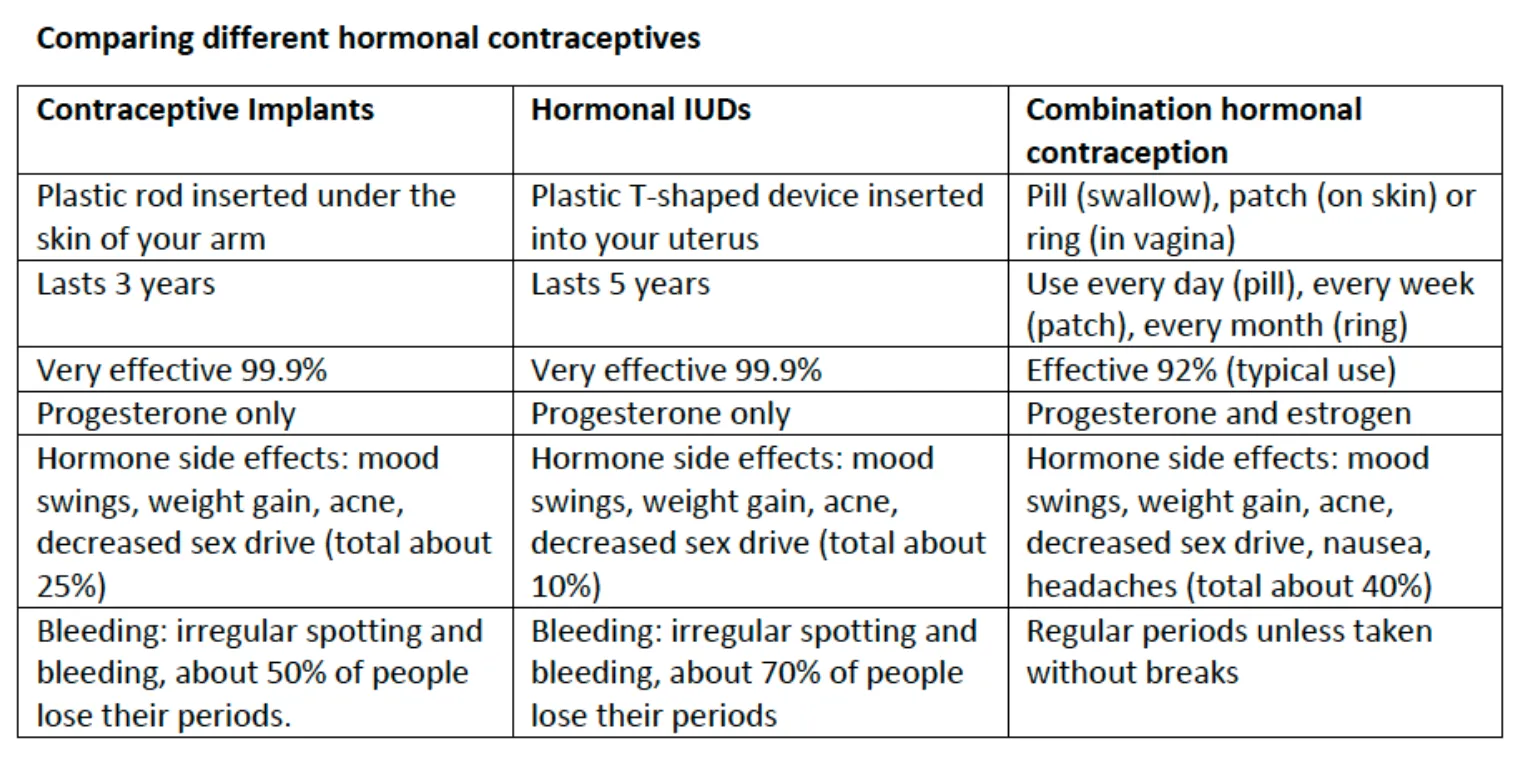
- Both methods are excellent forms of birth control.
Nexplanon ® is 99.95% and lasts for 3 years.
Hormonal IUDs are 99.8% and lasts for 5-7 years depending on the age it was inserted.
Copper IUDs are 99.2% effective and last 3, 5 or 10 years depending on the type. - IUDs are placed inside the uterus and impact the uterine lining while the subdermal implant (Nexplanon ®) is placed under the skin of the upper arm and works by inhibiting ovulation (release of an egg from the ovary).
- You will be able to predict your menstrual bleeding pattern with IUDs i.e. with a non-hormonal Copper IUD you will have a regular cycle whereas with a hormonal IUD you are more likely to have light spotting or no bleeding at all.
- With Nexplanon ® for most women, your period will stop or you might have infrequent bleeding . However, for a small percentage of implant users, periods could become unpredictable , longer, and/or more frequent.
- IUDs are placed inside the uterus and are very discrete.
- Nexplanon ® is placed under the skin of the upper arm. It is very discrete, yet it is still easy for you to feel under the skin of your arm with your fingertips. It feels like a small flexible rod about the length of a matchstick.
- Some women gravitate towards one form based on the type of procedure used to place the device, and other women might lean towards intrauterine (inside the uterus) versus subdermal (under the skin).
- Cost might be a factor.
- Generally Copper IUDs are the least expensive ( ~ $140), Hormonal IUDs cost ( ~ $430) and Nexplanon ® costs ( ~ $360).
- If you need further information, the experts at the IUD clinic in Langley would be happy to guide you.

- The Canadian Pediatric Society states that “long-acting, reversible methods of contraception should be the first-line birth control option for youth.” These methods have the lowest failure rate and are first-tier options.
- If you're not sure which IUD to choose or whether you should consider Nexplanon® Subdermal Implant, you are not alone.
- We are here to help provide you with the information you need to guide you , as well as assist you in gaining confidence in your contraceptive decisions.
- IUDs and Nexplanon® Contraceptive Implant, simply put, are the most effective non-permanent methods of birth control.
- Getting pregnant unexpectedly or at the wrong time in a woman's life can be very traumatic. Taking the big step towards effective contraception can allow you to focus on your personal and occupational goals, without any major surprises.
- The following position statements have been made by Canadian and International Societies regarding the use of IUDs and Nexplanon® Subdermal Implants:
- The Society of Obstetricians and Gynecologists of Canada (SOGC) and the American College of Obstetrics and Gynecology (ACOG), recommend Long-Acting reversible contraception as the first-line contraceptive choice for preventing pregnancy for all sexually active women.
- The Canadian Pediatric Society states that long-acting reversilbe methods of contraception ( IUDs or implant) should be the first-line birth control for youth as these methods have the lowest failure rate and are first-tier options.
- The World Health Organisation (WHO) recognizes reproductive and sexual health care as a fundamental human right.
